
 Jenny Smith Photography
Jenny Smith PhotographyHundreds of women who are “plunged into surgical menopause” are “being failed by the NHS”, says a menopause support campaigner.
Diane Danzebrink, 58, from Norfolk, has called for an urgent review of surgical menopause care to ensure all clinicians know how to prepare their patients.
Ms Danzebrink, who founded Menopause Support, said awareness had improved significantly, but “we haven’t seen change fundamentally to ensure every woman has access to good quality care at the time that she needs it”.
The Royal College of Obstetricians and Gynaecologists (RCOG) said it directed clinicians to comprehensive guidelines on surgical menopause produced by the British Menopause Society and the National Institute for Health and Care Excellence (Nice).
 Getty Images
Getty ImagesMs Danzebrink, who campaigned to put menopause education on the secondary school curriculum, called for comprehensive clinical guidance on surgical menopause for healthcare professionals.
It was made after she received 319 accounts from women who said they had not been told about the side-effects of having both ovaries removed.
“I read all 319 of those responses and there were several times when I was tearful to read about that much distress… it’s awful,” said the campaigner, who used to live in Buckinghamshire.
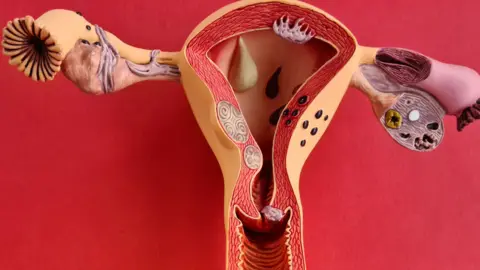
One example included a woman who had a hysterectomy aged 28, and by 31 she had severe vaginal atrophy, which was never spoken about.
Other women said they had waited more than a year to see specialists and could not afford to go private.
 Jenny Smith Photography
Jenny Smith PhotographyThe online Menopause Support survey of 521 UK-based women, aged 20-59, found 74.5% were not made aware, by health care professionals, of the side-effects of having both ovaries removed.
This included not being told that they could be plunged into premature menopause.
It also found 62% of those eligible for Hormone Replacement Therapy (HRT) said it was not discussed with them prior to having their surgery, with 36% being prescribed HRT immediately after surgery.
HRT is the first line of treatment for menopause symptoms.
Nice guidelines recommend people who have gone through premature menopause are offered HRT until the age of 50-51, by which time most women have experienced natural menopause.
‘Dumbfounded’
Ms Danzebrink, also is also part of the Make Menopause Matter campaign, said the results prompted her to search for clinical guidance for surgical menopause via the RCOG website, but could not find it.
She had hoped set guidance would ensure all health care professionals counselled patients fully, prior to surgery, and provided them with appropriate, ongoing care and support.
“I’m dumbfounded by the fact the organisation that represents the clinicians who are going to be removing ovaries doesn’t feel it needs either information for the public or guidance for clinicians,” she said.
“I think it is important to say in the last 10 years, things definitely are starting to move in the right direction.
“There’s more awareness and more information, but we need that information to be absolutely across the board, for all of our healthcare practitioners to be able to feel confident in their menopause knowledge.”
Dr Ranee Thakar, president of the RCOG, said it had a deliberate policy of avoiding the duplication of guidance to ensure consistency with established and nationally recognised guidelines.
“[It] makes it easier for clinicians to locate and follow the most reliable and relevant guidance and allows the RCOG to focus its efforts on areas where its contributions are most needed,” she said.
“Menopause and perimenopause symptoms can have an enormous impact on a woman’s life, and access to reliable, accurate education and information is crucial.”
She added that RCOG had a Menopause Hub and was updating its “Treatment for symptoms of the menopause” resource, which will include information about surgical menopause, and was part of an advisory group to develop a national menopause programme being led by a team at University College London.






